Choosing the Right UV Disinfection System for Hospitals
The hospital environment is a significant concern for patient health and safety as both a…
Illuminating the Future: UV Light Technology for Your Company
In an era where technology continually shapes how we live and work, UV (Ultraviolet) light…
3 Benefits of Automation in Environmental Service
Tell us if this sounds familiar: Your facility decides to double-down on its cleaning and…
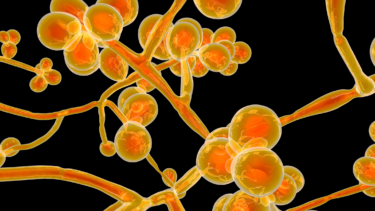
Use Case: Candida auris
In the spring of 2022, Candida auris was detected in the Emergency Department of a…
The Future of UV Disinfection Systems in Hospitals
Studies show that only 50% of surfaces in hospital rooms are sufficiently cleaned between patient…
A Day in the Life of a Computer Workstation
If you had to list the most urgent risks associated with environmental cleanliness in your…